[Article by Dr. Richard Malter, PhD.]
Original publication: Journal of Orthomolecular Medicine Vol. 16, No. 4, 2001]
Introduction
During the past ten years, we have read or heard about mothers who became violent and, in bizarre ways, killed one or more of their children. Many of these women were prescribed anti-depressants following the birth of a child and the onset of a post partum depression (PPD). In many cases, these mothers have been described as loving, caring, and well functioning women who were given prescriptions for antidepressant medications, especially one of the serotonin re-uptake inhibitor (SSRI) types such as Prozac® or Zoloft.® There is strong reason to believe that these SSRI anti-depressant drugs can radically alter the functioning of a person’s brain chemistry and lead to changes in thinking, emotional reactions, and behavior resulting in homicidal and/or suicidal violence.1,2 This type of un-maternal murderous behavior has been both shocking and baffling to many people. Because a plausible explanation of this appalling incomprehensible behavior is rarely, if ever provided, public reaction of both lay people and professionals to these murders is to vilify the mother. Even though there is well-documented evidence that many of these mothers were on SSRI anti-depressants and/or other powerful psychotropic drugs at the time of their crime, this fact is rarely if ever explored by journalists or other professionals. Psychiatrists hastily rush to the defence of their profession and its dependence on SSRIs and/or other powerful psychotropic drugs as the “standard of care” for depression. They are quick to deny that anti-depressant drugs can affect some people in such adverse ways.
Preventing PPD
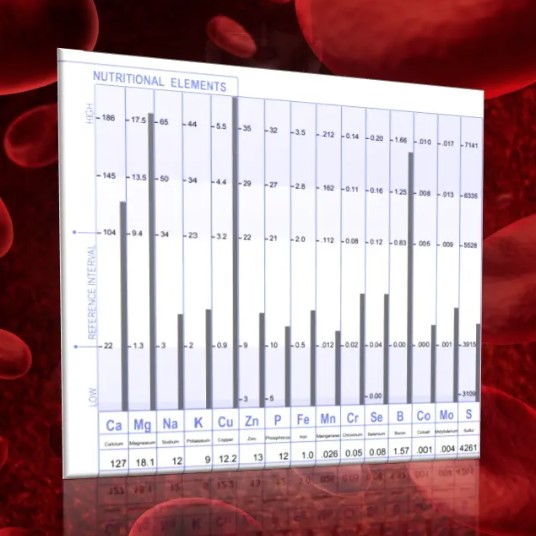
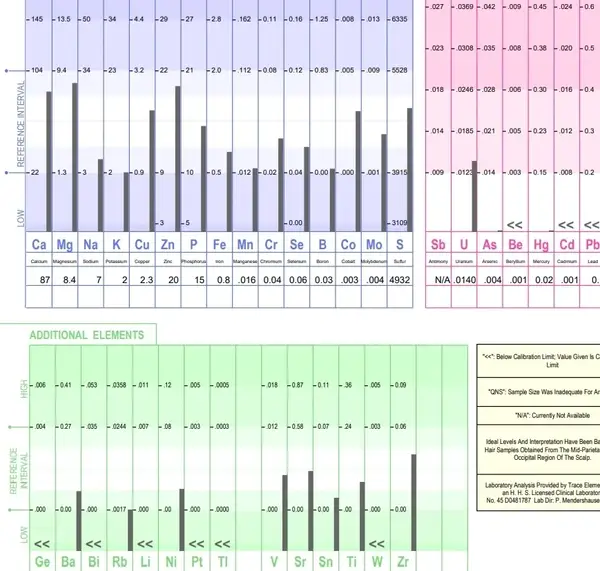
Since these are not isolated cases, it is critical that we address some important questions that relate to PPD and its treatment with toxic drugs that increase the risk of catastrophic outcome. In this context, are there underlying biochemical factors that predispose some women to experience clinically significant PPD? If so, what changes can be made in nutritional biochemical support in order to reduce the risk of PPD? Or, better yet, is it possible to use scientific nutritional interventions to prevent the clinical manifestation of PPD entirely? If we can reduce the risk of PPD or actually prevent the onset of this type of depression, then we can help new mothers avoid the exposure to these toxic SSRI drugs that are known to be associated with catastrophic violence. Bernard Rimland, Ph.D. described drug treatment as a “toxi-molecular” approach because the use of psychotropic drugs is inherently toxic by the very nature of their constituent toxic chemicals. The term “ortho-molecular” was applied by Pauling to describe nutritional treatments of psychological and emotional problems because these types of treatment tend to be corrective and more natural than introducing toxic drugs into a person’s system.3 Based on the clinical experience of this writer, there are data from hair tissue mineral analysis (TMA) that strongly suggest that excess copper and/or a low Zn/Cu ratio are major contributing factors to the risk of PPD.4,5,6,7 According to Pfeiffer, excess copper is related to [Continue reading full article here…]